.jpg)
Cancer treatments often damage a young woman’s ovaries — so if the chemo saves her life, she may still face the inability to conceive a new life later on.
Exciting research from Israel now reveals the mechanics of this heartbreaking problem and – most importantly — a long-sought-after way to avoid it.
In a study published in Science Translational Medicine (published by the American Association for the Advancement of Science), the authors describe how adding an Israeli-synthesized compound, AS101, to the chemotherapy regime successfully prevented infertility.
Doctoral student Lital Kalich-Philosoph and senior researcher Dr. Hadassa Roness used a mouse model of a common chemotherapy drug to understand how it attacks the ovaries and the eggs inside them.
Their research was done at the Center for Fertility Preservation at the Chaim Sheba Medical Center – Tel Hashomer Hospital in Israel, headed by Prof. Dror Meirow, in collaboration with the Cancer AIDS and Immunology Research Institute at Bar-Ilan University, headed by Prof. Benjamin Sredni.
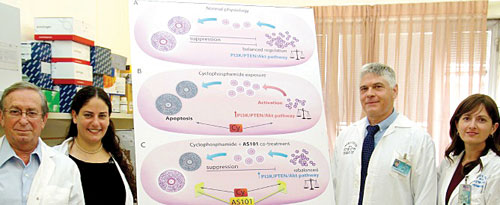
Meirow explained that doctors have long believed oocytes (egg cells) were destroyed as a direct result of the toxic chemotherapy. But the Israelis discovered that the treatment actually triggers an abnormal wave of growth in these dormant cells before killing them. The result is that the woman’s natural reserve of egg cells is depleted – a condition called ovarian burnout.
“This new understanding of the mechanism behind the loss of these cells has allowed us to shift the focus and find a new drug that can prevent the growth of the oocytes,” Meirow said.
Before this groundbreaking discovery, the only way to preserve fertility in female cancer patients has been extracting and freezing their eggs or ovarian tissue for transplantation after recovery. But this approach cannot be used for every patient. Moreover, it is invasive, expensive and carries no guarantee of success.
Researchers have long agreed that it would be far better to figure out how to prevent – or at least diminish — the damage and loss of eggs that occurs during chemotherapy. That’s what this Israeli study has done.
Restores natural balance in ovary
Once they understood what was happening in the ovaries of cancer patients, the researchers experimented with AS101 — a drug candidate developed by Prof. Michael Albeck at Bar-Ilan University and now in advanced clinical trials for use in cancer patients — to block the activation and growth of the dormant oocytes.
Egg cells in mice treated with AS101 in conjunction with chemotherapy remained dormant and survived the entire treatment. Later, these test mice had normal fertility, whereas the ones treated with the cancer drug alone had a lower rate of pregnancy and fewer total offspring.
As Kalich-Philosoph explains it, AS101 restores balance in the ovary, preserving the reserve of eggs by acting as an inhibiting factor on the burnout mechanism. “That’s why AS101 is a novelty to preserve fertility to cancer patients.”
Sredni said AS101 has shown “a very safe profile in clinical trials.” Adding it to the treatment cocktail does not make cancer treatments any less effective. In fact, it may even increase effectiveness by sensitizing tumors to anti-cancer drugs.
Future experiments will seek to translate results from mice into human patients and confirm the effectiveness of AS101 for preserving fertility in women undergoing chemotherapy.
The prize-winning study was supported by grants from the Kahn Foundation, Israel Cancer Association, Israel Ministry of Health, Dave and Florence Muskovitz Chair in Cancer Research, and the Jaime Lusinchi Research Institute in Applied Sciences. Hadassa Roness also is director of special projects at Hervana, Israeli developers of a non-hormonal, long-acting and non-invasive birth control solution.
Additional contributors to the study include Dr. Alon Carmely, Dr. Michal Fishel-Bartal, Dr. Hagai Ligumsky, Dr. Shoshana Paglin, Prof. Ido Wolf, and Dr. Hannah Kanety — all of the Sheba Medical Center.
Abigail Klein Leichman is a writer and associate editor at ISRAEL21c. Prior to moving to Israel in 2007, she was a specialty writer and copy editor at a daily newspaper in New Jersey and has freelanced for a variety of newspapers and periodicals since 1984.
By Abigail Klein Leichman Israel21c