
The expression “brain on fire” means that there is brain inflammation, as opposed to having a true psychiatric disorder where the disorder is only a symptom and not the disease. The distinction between primary and secondary mental illnesses is essential. Basically, “primary” means there is no cause for the mental illness other than the person’s nature. Whether it is suggested by the typical presentation of a well known mental illness or by a family history, primary psychiatric disorders have treatment but no cure. Even though one can achieve stability and control over symptoms with long-term use of drugs, this is not devoid of risk of side effects. Likewise, such drug use can limit one’s potential by affecting his/her genuine personality to a greater or lesser degree.
On the other hand, secondary psychiatric disorders are due to curable non-psychiatric diseases. Whether the treatment is long or complex, the goal is to uproot the psychiatric disorder by identifying and treating the root causes.
Non-Psychiatric Causes Of Mental Illnesses
The causes of neuroinflammation are numerous and often overlap each other. Many non-psychiatric diseases may cause psychiatric disorders. Aside from the classic examples of alcohol intoxication, drug abuse or hypoglycemia (low blow sugar) that may cause temporarily psychiatric disorders, the most common ones are toxoplasmosis, tick-borne diseases (including Lyme disease and co-infections), auto-immune encephalitis, mold toxicity, heavy metal toxicity, pesticides, histamine, glutamate, excess or deficit in copper, zinc, vitamin B deficiencies, porphyria, and mast cell activation syndrome (MCAS).
Lyme disease and tick-borne diseases are probably the most common causes of secondary mental illnesses in the northern states of the United States. According to psychiatrist Robert Bransfield, M.D, Lyme diseasemay be responsible for a wide spectrum of neuropsychiatric symptoms, which may include: developmental disorders, autism spectrum disorders, schizoaffective disorders, bipolar disorder, depression, anxiety disorders (panic disorder, social anxiety disorder, generalized anxiety disorder, OCD), intrusive thoughts, eating disorders, sleep disorders, addiction, cognitive impairment, brain fog, seizure disorders, suicide, violence, social withdrawal, depersonalization, dissociative episodes, derealization, etc. A psychiatric disorder may be the only symptom. Brian Fallon, MD, director of the department of Lyme disease at Columbia University, writes: “Psychiatrists who work in endemic areas need to include Lyme disease in the differential diagnosis of any atypical psychiatric disorder.”
Other causal factors for psychiatric disorders include autoimmune encephalitis. Commonly found in the pediatric population, it may also affect adults. They may overlap the tick-borne disease symptoms but are more remarkable by excessive OCD.
Heavy metals, mycotoxins released by mold and other environmental toxicants are neurotoxic and may also be responsible for neuropsychiatric disorders. Mercury may lead to emotional changes such as mood swings, irritability, nervousness, hallucinations and psychosis. Mycotoxins in children have been implicated in confusion, disorientation, brain fog, difficulty focusing, insomnia, anxiety, mood swings, irritability, depression and autism spectrum disorder.
Mold should be always checked for in the home, especially when two or more family members living under the same roof have a neurological and/or psychiatric disorder. Anxiety and depression may be common six months after COVID-19 recovery. Excessive glutamate release has been associated with the development of many major psychiatric disorders such as schizophrenia.
Excessive copper has been associated with paranoid schizophrenia, bipolar disorder, ADHD, autism and violent behavior, whereas low levels of copper is associated with oppositional disorder. Children with low selenium concentrations are more prone to anxiety, panic disorder, generalized anxiety disorder, social anxiety disorder and school phobia. Zinc deficiency can lead to depression, increased anxiety, irritability and emotional instability.
Deficiency of Vitamin B12 can result in neurological and psychiatric problems, such as irritability, changes in personality, depression and memory loss. Folate deficiency is associated with depression, schizophrenia, bipolar disorder, autism and ADHD. Histamine plays an essential role in the regulation of neuropsychiatric disorders such as anxiety, depression, panic and schizophrenia. Histamine affects cognition, emotion and behavior. Food high in histamine and mast cll activation syndrome may cause an overload of histamine. Gut inflammation can also cause cognitive and mental health disorders.
Clues for Psychiatric Causes Of Mental Disorders
Family history of psychiatric disorders and the presence of such disorders in multiple family members, even more so with the same mental disorder, of course provide a strong clue for the likely presence of mental disorders in patients.
Clues for Non-Psychiatric Causes of Mental Disorders
Ultimately, the goal is to prove that behind a diagnosis of psychiatric disorder – even though the individual might meet all the diagnostic criteria of a known psychiatric disease is the possibility that a curable disease may be at the root of it. Why? Because it is the only chance to convert a lifelong disease into a short and curable one. The more evidence we have to find toxins in excessive amounts and infections known to cause psychiatric disorders, the more plausible is the hypothesis that the psychiatric disorder is due to something other than psychiatric causes. Aside from clinical clues, it is essential to collect objective data like brain Neuroquant MRI and inflammatory markers that prove there is inflammation, and in particular brain inflammation. By itself, objective data does not allow any diagnosis as it is not specific. It can, however, challenge a diagnosed psychiatric disorder and monitor the progress under treatment. Clues from objective data include:
Absence of family history.
Atypical mental disorder.
The absence or the poor response to psychiatric medications.
Presence of other symptoms other than emotional, cognitive or behavioral.
The presence of non-psychiatric symptoms like muscular or joint pain suggests that mental disorder may not be the disease but only symptoms of a more complex disease. How to explain other symptoms? How will the orthopedist explain unexplained sweats, intrusive thoughts and depression? How will the neurologist explain abdominal pain, anxiety or migratory joint pain? You may realize that there is probably a common denominator if only one connected the dots:
Evidence of infections known to cause mental disorders
Evidence of toxicity known to cause mental disorders
Evidence of inflammation by the presence of markers of inflammation: MMP:9, TGF:beta1, Interferon:ALPHA, EIA, Interleukin, Cardiolipin antibody, TNF, VEGF, Serum, Complement C4a (activated), ESR, CRP, and CD57 panel absolute HNK1.
Evidence of inflammation on brain MRI Neuroquant
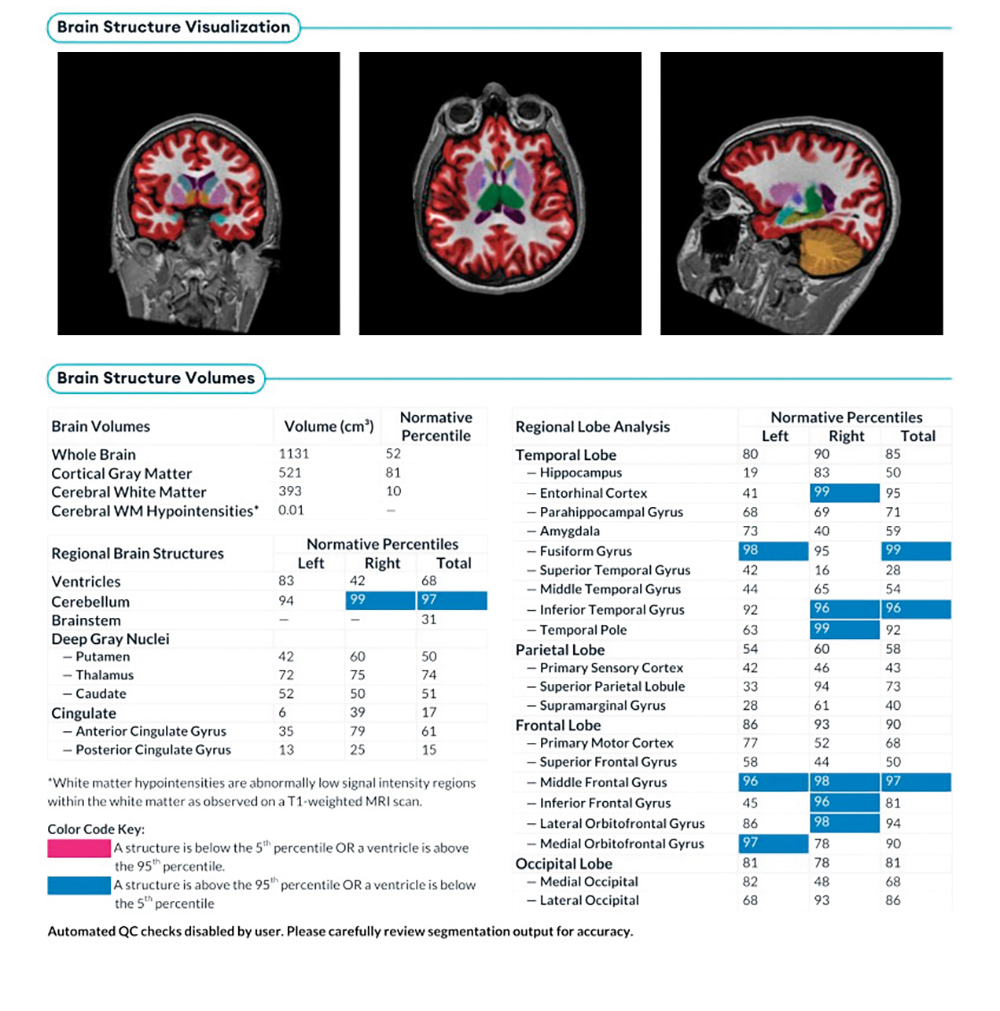
The Neuroquant MRI consists of the computerized measuring of the size of each part of the brain in cm3, which increases reliability. This allows a very precise appreciation of subtle hypertrophy and of atrophy that may not be picked up by the naked eye of a radiologist. The presence of hypertrophy is evidence of inflammation.
An Actual Case
An 18-year-old teenager suddenly developed a change of personality. The teacher called the parents, concerned about obvious mood swings, with a severe depressed mood contrasting some other days with hyperactivity. The patient wanted to learn but could not. He had brain fog, memory impairment and difficulty focusing but his symptoms were joint pain, headaches, chronic fatigue, bone pain and dizziness. What could have been understood as a new psychiatric disorder was actually brain inflammation. He was found to be positive for a tick-borne disease. Below is the picture of his brain Neuroquant MRI. he parts of his brain(indicated in blue on the chart), of which 95% of the population’s percentile is less than his, h is considered as hypertrophy and therefore as inflammation.
Alain Mass, MD is board certified in Family Medicine and a member of the International Lyme and Associated Diseases Society (ILADS), a diplomate of the International Society of Environmentally Acquired Illnesses (ISEAI) ana member of the Pandas Physician Network (PPN). He can be reached at (845) 623-0047 or [email protected]












