It’s clear that the COVID-19 pandemic has affected so many people and changed how people interact and work. We are living in a time where traditional workplace cultures and practices have to be adapted to our “new normal”—wearing face masks, practicing social distancing, new sanitation protocols and telecommuting, among other health and safety concerns. The workplace as we know it has changed!
With the current disturbance, businesses may lose focus on keeping up with compliance requirements, which can be a huge mistake. Companies must continue to stay compliant with policies and procedures. Here are the latest legislative and compliance regulations.
No Surprises Act is a vital part of the the Consolidated Appropriations Act (CAA). This will not go into effect until 2022. The No Surprises Act applies to emergency and post-stabilization care and nonemergency care in in-network facilities. It applies to fully insured as well as self-funded plans. This also includes air ambulance services; and an advisory committee is to study ground ambulance services. This will limit a consumer’s out-of-pocket maximum to their in-network cost-sharing, including deductibles and copays. So this is consumer protection at its best. On top of that, providers and facilities cannot balance-bill patients.
Hospital Price Transparency went into effect on January 1, 2021. This is very different from the No Surprises Act. The Hospital Price Transparency rule makes it very clear that each and every hospital in the U.S. will be required to provide clear, accessible pricing information online about the items and services they provide. They can provide this by a comprehensive machine-readable file with all items and services or in a display of shoppable services in a consumer-friendly format. The information hospitals are required to post include:
Billed charges;
Minimum and maximum negotiated rates with insurance carriers;
Cash price for people who do not have insurance.
There are potential penalties in place for hospitals that do not comply. This will make it easier for consumers to shop and compare prices across hospitals and estimate care costs. The Centers for Medicare and Medicaid Services (CMS) plans to audit a sample of hospitals in addition to investigating complaints that are submitted to CMS.
Consolidated Appropriations Act of 2021 (CAA). It passed on December 21, 2020 and was signed by President Trump on December 27, 2020. The CAA includes $900 billion in COVID-19 relief. Employers can choose to extend the Families First Coronavirus Response Act (FFCRA) Emergency Paid Sick Leave and Emergency Family Leave benefits, but it’s not mandatory.
COVID-19 Relief
Economic relief is a stimulus check of $600 for individuals making up to $75,000 per year and $1,200 for couples making up to $150,000 plus an additional $600 per dependent child under 17 years old. Payments would be based on 2019 taxes. If you haven’t received your check yet, go to the IRS website for assistance.
Paid leave credits also extend the credits for paid sick and family leave under the second COVID-19 relief package through March 31, 2021. However, it does not extend FFCRA. There is $284.5 billion for the first and second forgivable Paycheck Protection Program (PPP) loans. Small businesses can receive a second PPP loan if they have less than 300 employees and demonstrate a revenue reduction of 25%. The maximum loan amount is $2 million. Also, premiums for dental and vision insurance are covered under payroll costs.
In addition, The House voted Saturday, February 27, 2021 to pass President Joe Biden’s $1.9 trillion COVID-19 relief package. This bill includes $1,400 direct payments; a $400-a-week federal unemployment bonus; a per-child allowance of up to $3,600 for one year; and billions of dollars to distribute coronavirus vaccines and to assist schools and local governments. The $1,400 checks would be sent to individuals who make up to $75,000 a year or married couples making $150,000, and payments would gradually decrease for those who make more, zeroing out at $100,000 for individuals and $200,000 for couples.
Finally, employers should review their plan documents to confirm that they include the below required changes:
Confirm that your group health plan’s out-of-pocket maximum complies with the Affordable Care Act’s limit for 2021. Under the ACA, an Applicable Large Employer’s coverage is considered affordable if the employee’s required contribution to the plan does not exceed a certain percentage of the employee’s household income for the taxable year. For plan years that begin on or after January 1, 2021, the affordability percentage is 9.83%.
Confirm that the health insurance plan’s deductible and out-of-pocket maximum comply with the 2021 limits. Health plans are subjected to limitations on cost-sharing
for essential health benefits. The annual limit on cost-sharing for essential health benefits for plan years beginning on or after January 1, 2021, is $8,550 for self-only coverage and $17,100 for family coverage. This doesn’t mean you have to choose a plan with this maximum out-of-pocket.
Preventive care services are required to be offered without imposing cost-sharing requirements. Also, the ACA sets a dollar limit on employees’ salary reduction contributions to a health flexible spending account (FSA). Employers may impose their own dollar amount on employees’ salary reduction contributions to a health FSA account, as long as the limit does not exceed the ACA’s maximum limit in effect for the plan year. The IRS has not yet announced the limit for 2021 plan year for FSAs.
Lastly, provide all participants with a summary of their benefits and coverage. The ACA requires employers to provide a Summary of Benefits and Coverage (SBC) to applicants and enrollees to help them understand their coverage and make coverage decisions. Employers must provide the SBC to participants and beneficiaries who enroll or re-enroll during an open enrollment period.
The Bottom Line
Make sure your business is updated with all compliance regulations. In any case, don’t just sit back and allow a premium increase. There may be better plans with benefits that better suit your needs. Just give Cosmo Insurance Agency a call. We will simplify the process for you and ensure you are compliant.
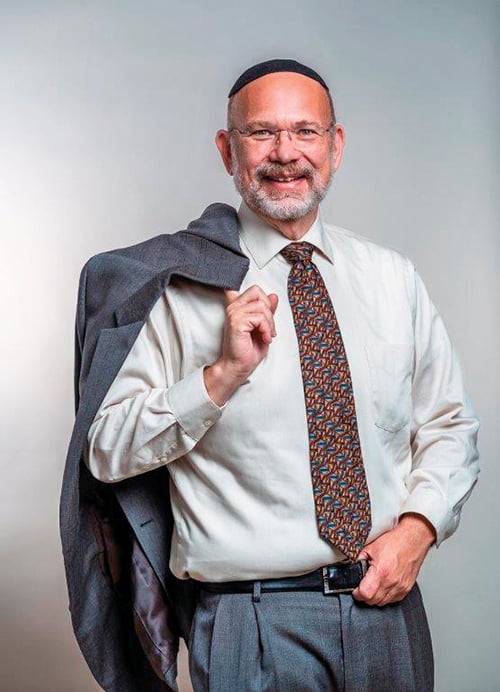
Mark Herschlag is the founder and CEO of Cosmo Insurance Agency, which is based in Ocean County. Cosmo Insurance Agency offers personalized solutions for individuals and businesses looking to obtain health, life, dental, long term care or disability insurance. For more information or for a free, no-obligation quote, please call (201) 817-1388 or email: [email protected].