
Part 1
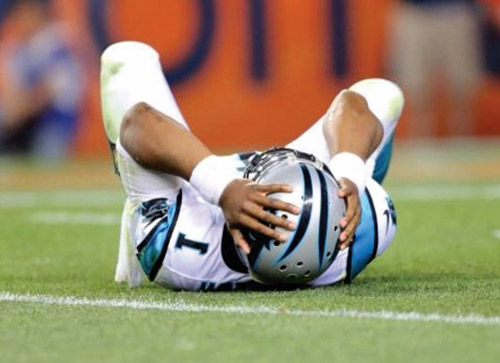
Nate goes for the goal, the opponent’s defense kicks the ball and BAM! Nate takes a massive hit to his head. He falls down grabbing his head. The play stops and the coaches run over. Nate slowly gets up and walks to the bleachers. The crowd and other players applaud their support. Should Nate go back in the game? He says he’s fine. The coaches look at him and see that he seems a little out of it, but since he says he’s fine, they don’t want to keep him on the bench…what is the right call to make?? Should Nate play or sit out? How long are they going to keep him benched? What if his parents get upset that their son wasn’t put back in? The team is counting on their star player to help them win this game…
What is a concussion?
A concussion is a brain injury, often referred to as a mild traumatic brain injury, that results in a cascade of changes that cause an energy crisis in the brain. This alters the way the brain functions. It can be caused by a direct blow to the head or an indirect force that causes a jolt to the body or head. The brain undergoes a rapid acceleration/deceleration or a rotational force depending on the blow that has occurred. Loss of consciousness may occur, but most often does not, which makes it difficult to recognize when a concussion has been suffered.
How can you recognize a concussion?
The diagnosis of a concussion is based on patient report of symptoms and observable signs that are reported by family members, teammates, coaches or others close to the individual. A medical professional with experience in concussion management will take a detailed history (interview) and perform testing to make a diagnosis.
What the patient may experience can fall into four categories of symptoms: physical, cognitive, emotional and sleep behavior.
Physical symptoms include headache, dizziness, fatigue and sensitivity to light, among others.
Cognitive symptoms can include memory problems, especially as related to just before or after the injury occurred; feeling slow mentally; or confusion.
Emotional symptoms can be mood swings or irritability.
Sleep changes might be an increase or decrease in sleep or difficulty falling asleep.
Symptoms may or may not start immediately after a blow occurs and are frequently delayed. This is a critical point. Especially in sports-related injuries, the athlete may not feel the full effect of the injury in the moment that it has occurred. It can take minutes, hours or even days for symptoms to manifest. Knowing what to watch for after an injury can make all the difference in identifying when a concussion has been suffered. Sometimes symptoms do not start until there is a return to daily activities that require a lot of thinking or physical exertion. Remember, a concussion results in an energy crisis in the brain. Activities that tax the brain, either cognitively or through increased physical demand, can exacerbate or bring on symptoms that had not been observed or noticed earlier.
Observable signs at the time of injury include dazed or stunned appearance, confusion about the game, score, opponent or the last play, moving in a clumsy way, difficulty with recall of events just before or after the hit or loss of consciousness. One of the ways to quickly assess if the individual is affected is to check the person’s orientation by asking questions that should be easy to answer, such as day of the week, president, year or score of the game. Loss of consciousness and vomiting do not always occur and should not be relied on as the only indicators of concussion. Parents or friends may also observe behavior changes like extreme irritability. Cognitive impairment may be observed if a family member notices that the individual has a slower reaction time or difficulty concentrating. Drowsiness and disruption of normal sleep patterns may also be observed.
What can you do?
First and foremost, if a concussion is suspected, the rule is, “when in doubt, sit them out.” This adage is used for sport-related injuries to help coaches and teammates support the safety of players. If a player sustains a blow, the player must immediately be sidelined and monitored for signs and symptoms. If a child falls off playground equipment, the same rule applies. When an injury occurs, the injured person must be assessed to determine whether or not a concussion has been sustained. As stated above, symptoms can be, and often are, delayed in onset. It is important to allow a person who may have been concussed the time to sit out and be monitored.
Youth athletes and their teammates need to be well informed of what to look for, and the importance of looking out for each other. There is nothing more powerful than team support when an athlete has to make a decision about reporting how they feel and reporting with complete honesty.
Many times parents bring their children to the emergency room. At the ER, the patient will be assessed for skull fracture or bleeding in the brain, or other potentially more life-threatening injuries as well as for concussion. It is important to know that an ER visit is necessary at times, such as if there is repeated vomiting, loss of consciousness longer than 30 seconds, a headache that gets increasingly painful over time, dilated pupils or slurred speech.
More commonly, parents contact the pediatrician. Sometimes a doctor is comfortable giving advice over the phone and other times an office visit is advised. If your child is hurting enough for you to make that call to the doctor or to bring the child in to see the doctor, you are more than likely dealing with a concussion. Following a visit to the ER or pediatrician, parents can then face the question: Concussion diagnosis is made. Now what???
Next week the topic of how to handle concussion for best recovery will be presented.
By Danit Macklin PT, DPT, ITPT
Danit Macklin PT, DPT has a doctorate degree in physical therapy as well as advanced certification in vestibular and concussion testing and treatment. She has been affiliated with Hackensack University Medical Center for over 10 years in the pediatric physical therapy department where she provides inpatient care in the Neonatal and Pediatric Intensive care units as well as outpatient services. As there were no post-concussion treatment centers providing care to patients with prolonged symptoms and diagnoses of post-concussion syndrome, Dr. Macklin is pleased to now be offering these specialized services. She can be reached at the Balance & Concussion Therapy Center, 551-888-2282 or at her website mybalancecenter.com.