I hear this multiple times per week.
A patient comes into the office with pain along the outer aspect of the elbow where they don’t know what injury caused the pain and only have a vague recollection of when it started. Usually they will say that the pain is made worse with such things as lifting a milk carton out of the refrigerator and will often reveal that it is aggravated with working out. Most times, they will present after the pain has been ongoing for at least six weeks. And almost always, after a brief physical exam and with a few questions answered, I conclude the problem to be a condition known medically as lateral epicondylitis, more commonly referred to as tennis elbow.
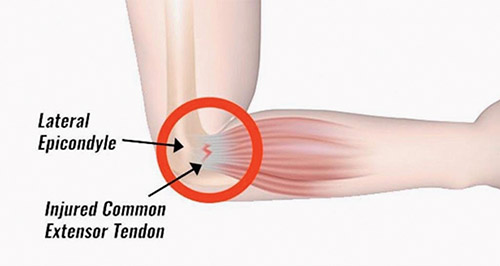
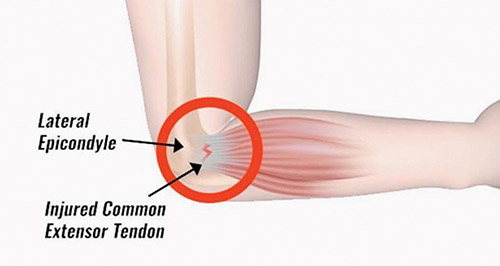
The development of tennis elbow has nothing directly to do with playing tennis or any racket sports. Instead it results from repetitive traumatic overload of the tendinous origins of the muscles in the forearm that extend the wrist and sometimes additionally the fingers. This repetitive overload has the potential to cause small microscopic tears in the tendon that are unable to effectively heal. The reason for this inability to heal is the diminishing blood supply to tendons as we age. Oddly enough, our bones have robust blood supply throughout our lives, but the same cannot be said for the tendinous insertions where our muscles attach to bones. There’s always a balance between tendinous injury from overuse and our innate healing response, and unfortunately, as we get older, this balance tips in favor of lack of complete healing and microtendinous injury. This is tennis elbow. This disease process has been characterized further by looking at the tendons of folks with it under the microscope. What is seen is a disorganized array of the collagen fibers that should otherwise be aligned parallel as in normal tendons. Further, there is an influx of disorderly vascular channels perhaps as an attempt by our body to deliver more blood supply for healing. Lastly, there is an increase in nerve endings. The combination of these three factors, known as angiofibrous dysplasia, is what is responsible for the development of painful tennis elbow and is also why it peaks in people in the fourth through sixth decade of life.
The good news regarding tennis elbow is that it is a self-limiting condition, meaning that the pathologic process in essence runs its course and ultimately becomes less symptomatic. However, in the severe form of it, this can take over a year. That is why everything the treating orthopedic surgeon can offer is geared at speeding up this time frame to resolution. There are a lot of treatment options out there ranging from anti-inflammatory medication, to physical therapy, to brace use, to injection therapy and, lastly, surgery. In my opinion, the vast majority of patients respond well to physical therapy combined with brace wear. The therapy exercises utilized focus on eccentric strengthening of the forearm muscles involved. Eccentric strengthening versus concentric strengthening is when the muscle is being activated but is lengthening as it is fired, whereas concentric strengthening is when the muscle is activated while shortening, which is how most would envision a muscle firing. This eccentric firing of the muscle is believed to stress the tendon origin and promote healing at the site of tennis elbow. Wearing an immobilizing wrist brace at night is also very helpful, as how people position their wrist when they sleep can aggravate this condition. Injection therapy ranges from the use of steroids to platelet rich plasma (PRP); both have been documented to show benefit in well-designed studies. Ultimately, if all else fails, surgery is an option and involves the exploration of the diseased tendon with either removal of the poorly functioning angiofibrodysplastic tissue or the same combined with tendon repair.
Tennis elbow, medically referred to as lateral epicondylitis, is a condition that is almost a rite of passage in that it affects a large portion of the population at some point in their lives. Ultimately, it is quite treatable and this is where your local sports medicine orthopedic surgeon can help!
Dr. Heitman is board certified with the American Board of Orthopedic Surgery and is a fellow of the American Academy of Orthopedic Surgeons. He also maintains memberships in the Arthroscopy Association of North America and the American Orthopedic Society for Sports Medicine, attending yearly conferences and surgical labs to stay abreast of the latest operative solutions and techniques. He holds medical licenses in the states of New York, New Jersey and California.